Energy for Health, Vol. 24, 2024
Kanogwan Kimram1, Naruemon Plongthong1, Warangkana Promsatit1, Napat Kaewduangjai1, Pakawan Asawawongsawat1
1 Intensive care unit, Kasetsart University Veterinary Teaching Hospital, Faculty of Veterinary Medicine, Kasetsart University, Bangkok, Thailand
Introduction
Traumatic condition in critical cases have a strong ongoing relationship. Magnetic therapy is one of the non-invasive complementary therapies. It is a safe, and easy method to directly treat the site of injury, the source of pain and inflammation, and other types of disease. Magnetic therapy was applied to promote bone healing (1), treat osteoarthritis (2) and inflammatory diseases of the musculoskeletal system (3), alleviate pain, and may have benefits to enhance healing in traumatic cases.
The purpose of this case report was to describe the positive outcome to use the electromagnetic therapy for complementary rehabilitation therapies with conventional treatments of a dog in multiple trauma conditions.
Case Report
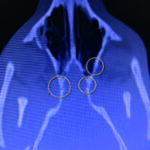
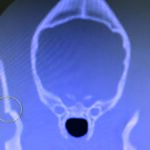
This case study involves a 5-monthsold, intact male Golden Retriever dog presented with tetraparesis, seizure and comatose by a car accident 5 days ago. Physical examination presented unconsciousness, tetraparesis, tachypnea, right temporomandibular joint (TMJ) luxated and crepitus of left humerus. Neurological examination was localized to cerebral cortex and brain stem lesions. The Modified Glasgow Coma Scale (MGCS) was 3. Laboratory tests revealed anemia of 23.1% (reference range, 35-45%), leukocytosis of 19.09 x 103/μL (reference range, 5-14.1 x 103/μL). Radiography was presented to skull fracture, lung hemorrhage (Figure 1) and left humerus fracture (Figure 2).
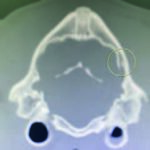
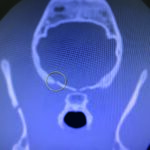
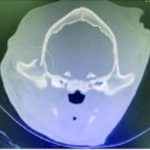
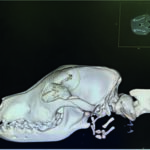
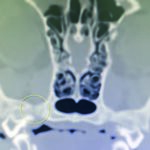
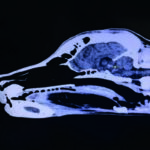
CT scan of skull is preferred for evaluate bone fractures and identify areas of acute hemorrhage or edema. CT scan showed multiple sites of skull fractures, right maxilla, both frontal, right zygomatic, right caudal mandible, right caudal zygomatic, right temporal, left occipital bone (Figure 3) and patchy small area of hyper-attenuation at the cranial of midbrain in pre-contrast study (Figure 4), no detectable mass effect, hypo-attenuated of large edematous parenchyma in the brain, right temporomandibular joint is displacement (Figure 5) and left tympanic bulla shows partial ventral fluid-filled.
CT skull presented to multiple skull fractures, brain edema, midbrain hemorrhage and right TMJ luxation.
Brainstem auditory evoked response (BAER) was performed under coma conditions presented to both intact brain stem activity and decreased amplitude at left brain stem.
Figures 3.1, 3.2, 3.3, 3.4, 3.5, 3.6, 3.7
Figures show multiple sites of skull fractures, right maxilla, both frontal, right zygomatic, right caudal mandible, right caudal zygomatic, right temporal, left occipital bone.
Figures 4.1, 4.2
Patchy small area of hyper-attenuation at the cranial of midbrain in pre-contrast study.
Materials and Methods
The treatment plan focused on maintaining vital signs through supportive care, including pain medication, antiepileptic drugs, antibiotics, oxygen supplements, and blood transfusions.
Surgery was not an option due to the high risks associated with general anesthesia.
After three days of treatment, electromagnetic therapy was added. The patient received pulsed electromagnetic field (PEMF) therapy twice a day using the PMT QS device (ASA Srl, Arcugnano, Italy), using the portable solenoid applicator (Ø-50cm), following the neuromuscular disease pre-set protocol (Frequency: 25 Hz, Intensity: 15%, Treatment duration: 20 min, Magnetic flux density: ~7.5 G).
Results and Conclusion
After 3 days of electromagnetic therapy, the patient’s MGCS improved, and he began eating independently. The patient was discharged from the intensive care unit after one month, exhibiting an overall improvement in clinical and neurological signs, as well as a Modified Glasgow Coma Scale (MGCS) score of 14. (Figure 6)
Subsequently, the left humerus underwent callus formation at the fracture site (Figure 7), thereby enabling the patient to regain ambulatory capacity and consciousness.
In conclusion, the use of electromagnetic therapy as a complementary treatment for multiple organ trauma and traumatic brain injuries with low MGCS has been demonstrated to be an effective approach. Therefore, this may represent a novel approach for critical care patients with complex conditions that are refractory to conventional therapy.
One advantage is that the treatment is safe and does not disrupt the delicate physiological state of the patient.
Figures 6.1, 6.2, 6.3, 6.4
Clinical condition of the subject at baseline, during a PEMF session, along hospitalization and at discharge visit.
Figures 7.1, 7.2, 7.3
Fracture evolution during the PEMF treatment.
Bibliography
Peng, L., Fu, C., Xiong, F., Zhang, Q., Liang, Z., Chen, L., … & Wei, Q. (2020). Effectiveness of pulsed electromagnetic fields on bone healing: A systematic review and meta-analysis of randomized controlled trials. Bioelectromagnetics, 41(5), 323-337.
Cianni, L., Di Gialleonardo, E., Coppola, D., Capece, G., Libutti, E., Nannerini, M., … & Vitiello, R. (2024). Current Evidence Using Pulsed Electromagnetic Fields in Osteoarthritis: A Systematic Review. Journal of Clinical Medicine, 13(7), 1959.
Kull, P., Keilani, M., Remer, F., & Crevenna, R. (2023). Efficacy of pulsed electromagnetic field therapy on pain and physical function in patients with non-specific low back pain: a systematic review. Wiener Medizinische Wochenschrift, 1-9.