Plantar fasciitis
is the most common cause of heel pain and is responsible for up to 15% of all foot symptoms requiring medical care in the adult population. MLS® Laser Therapy has been shown to be safe and effective in treatment of painful orthopedic conditions, although no randomized controlled studies have evaluated its efficacy for the treatment of chronic plantar fasciitis.
The Effects of a Class IV Multiwave Locked System Laser (MLS) on Plantar Fasciitis
J. Geldwert DPM
R. Minara DPM
The Center for Podiatric Care and Sports Medicine
111 East 88th Street, New York, NY 10128
ABSTRACT
Plantar fasciitis is the most common cause of heel pain and is responsible for up to 15% of all foot symptoms requiring medical care in the adult population. The MLS Laser Therapy has been shown to be safe and effective in treatment of painful orthopedic conditions, although no randomized controlled studies have evaluated its efficacy for the treatment of chronic plantar fasciitis. The MLS Laser is a class IV laser composed of a synchronized continuous emission (808nm) and pulsed emission (905 nm). This synchronization with a higher energy laser has been shown to have analgesic, anti-inflammatory and anti-edema effects.
The purpose of this study was to determine the effects of MLS Laser Therapy on patients suffering from plantar fasciitis. Twenty subjects with at least a one-month history of plantar fasciitis were enrolled in a randomized, non-placebo controlled study. The patients’ pain level on VAS and fascial thickness (as measured by sonography) were measured prior to treatment. Each patient was treated at the same location using the multi-diode hand piece at 700Hz, 218.4J three times a week for two weeks (6 treatment sessions total). Each treatment session lasted 7 minutes. Patients were then evaluated at 4, 8, and 12 weeks post treatment. At least 4 weeks, post laser therapy, patient pain level decreased from an average of 6.2 on VAS (range from 3-10) to 2.6 (range of 0-6). Sixteen of twenty patients reported decrease in pain levels. Fascial thickness decreased from .48 to .43 cm as measured via ultrasound. While fascial thickness did not decrease significantly, 80% of patients reported improvement in symptoms with an average decrease in VAS of 3.6.
INTRODUCTION
One of the most common ailments treated by foot and ankle specialists is plantar fasciitis. As the leading cause of heel pain, studies have shown that plantar fasciitis is responsible for upwards of 15% of all foot symptoms requiring medical care in the adult population (1). Outdated theories asserted that the aging, sedentary population was most commonly afflicted. However, we now know it is a condition that seems to affect a multitude of patient populations regardless of age, gender, race, weight, activity level or foot type. Some patients experience self-limiting symptoms, usually within one year. Many, however, seek treatment due to the severity or chronicity of pain. Typical conservative therapies for plantar fasciitis focused on stretching, proper shoe gear and orthotics, as well as therapies targeting inflammation; oral or topical NSAIDs, oral steroids, and very commonly, corticosteroid injections.
Some patients eventually opt for surgical intervention, due to lack of response to non-surgical therapy. The gold standard operative procedure is the fasciotomy, although other procedures have gained traction including radio-frequency coblation. Advanced therapies, including extra-corporeal shockwave therapy, have been shown to have positive effects on decreasing pain and increasing patient function (1).
Laser light therapy, specifically class 3B low-level laser therapy (LLLT) has been used extensively and studied in medical literature many times since its FDA approval in 1996. Bjordel et al performed a systematic review of over 200 randomized controlled studies on LLLT (2). There is strong evidence that LLLT improves angiogenesis, modulates biochemical inflammatory markers, increases growth factor secretion and increases collateral vessel formation (2). However, LLLT was ineffective in several studies as it had several limitations. The biological processes generated by laser/tissue interaction are mainly photochemical and are limited to a surface bio-stimulation. LLLT required long treatment times with numerous treatment sessions. Therapeutic results were achieved only at the end of the treatment period, and the treatment was only effective for pathologies at a certain tissue depth.
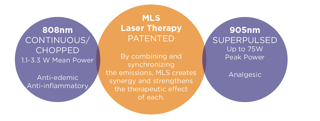
The MLS Therapy Laser is a class IV device composed of a synchronized continuous emission (808 nm) and pulsed emission (905 nm). This synchronization, combined with a higher energy output has been shown to have analgesic, anti-inflammatory and anti- edema effects, and is able to penetrate to more substantial tissue depths to treat a variety of pathologies.
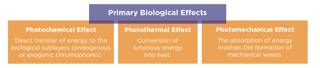
The biological interactions and therapeutic effects of the MLS Laser include the photochemical effect, the photo-thermal effect, and the photomechanical effect. The photochemical effect of the 808 nm wavelength increases the activity of the mitochondrial respiratory chain falling in the secondary absorption peak of cytochrome oxidase. The 905 nm wavelength increases the activity of mitochondrial respiratory chain complexes I, II, III, and IV as well as succinate dehydrogenase. This overall increase in the activation of mitochondria serves to increase the synthesis of ATP, potentially accelerating the healing process (3).
The photo-thermal effect increases biochemical reaction speed and tissue metabolism, as well as moderates vasodilation and decreases fluid viscosity. This leads to increased blood flow with decreased tissue rigidity, activating the inflammatory repair process while producing a generalized soothing, analgesic effect (4).
The laser light and photo-thermal effect leads to a photomechanical effect which causes forces which can act on both cellular and extracellular matrix (ECM) components of various tissues. The generation of these non-destructive, mechanical effects occurs through reversible deformation of the ECM. These forces help lead to cell growth and differentiation, protein synthesis, and ECM production. These actions aid in the maintenance of homeostasis of tissues with structural function like connective tissue, muscle, bone, and cartilage, essentially helping to regulate the tissue repair process. (5)
The MLS Therapy Laser has been shown to be safe and effective in treatment of painful musculoskeletal conditions, such as in Dr. Andrew Rader’s study on the effect of MLS on diabetic peripheral neuropathy (9). However, no studies have evaluated its efficacy for the treatment of chronic plantar fasciitis. The purpose of this study was to determine the effects of MLS Laser Therapy on patients suffering from plantar fasciitis.
MATERIALS & METHODS
Twenty patients from a single office were enrolled in the study. There were 11 female and 9 male subjects ranging in age from 32-80 with an average age of 42.5 years. Patients were included on the basis of a physical exam positive for typical findings of plantar fasciitis including pain on palpation of the medial calcaneal tubercle and/or plantar central heel at the fascial origin, pain along the proximal one-third of the fascial band and pain typically occurring after periods of rest.

Patients were required to have at least a one-month history of plantar fasciitis. Prior treatments did not exclude patientsfrom the study, unless they had received a steroid injection or anti-inflammatory medication within a month of initiation of laser therapy. Other exclusion criteria included pregnancy, epilepsy, and those patients with pacemakers.
The same practitioner treated all patients in the same office with the same MLS Mphi5 Laser using the same protocols. Each patient was treated for 7 minutes per session (700Hz, 218.4J) via the handheld diode over the area of chief complaints and typical trigger points. Settings were predetermined for tendinitis. Patients were treated two times a week for three weeks for a total of six sessions. Pain was determined prior to initiation of treatment via VAS. The patient’s plantar fascia was also measured via ultrasound. Average VAS rating prior to treatment was 6.2 ranging from 3-10, and the average sonographic measurement of the plantar fascia was 0.48 cm ranging from 0.19-0.71cm.
RESULTS
Upon completion of treatment protocols, patients were evaluated at 4, 8, and 12 weeks post treatment. All patients were evaluated at 4 weeks post-treatment, while only eight were evaluated at eight weeks, and only six at twelve weeks. At each post-treatment visit, patient pain level was determined via VAS, and new ultrasound measurements of the fascia were taken.
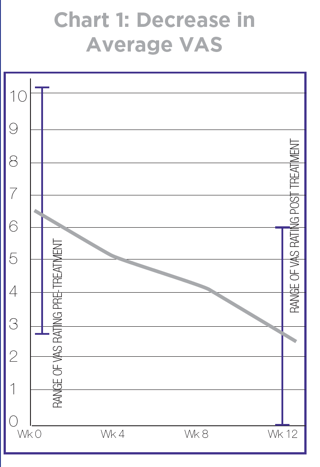
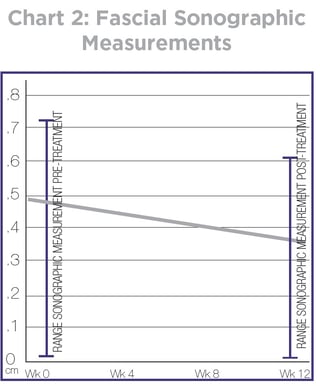
Average post treatment VAS was 2.6 (ranging from 0-6) with a significant average decrease of 3.6 (Chart 1). Eighty percent of subjects (16/20) reported a decrease in symptoms. Average fascial sonographic measurements minimally decreased from an average of 0.48 mm to an average of 0.43 mm (Chart 2).
DISCUSSION
Eighty percent of patients in the study reported decreased symptoms four weeks after treatment. While the fascial insertion also decreased in overall thickness, there was only a 0.5mm average decrease. However, there were some limitations to the study. Ideally, the patients would have had no prior treatments to better study the effects of MLS Laser Therapy as an isolated front line treatment for plantar fasciitis. Patients in this study had many prior treatments, and although they were excluded if any medical treatments (i.e. injections or oral medications) had been used in the past month, many patients continued to stretch and use custom or pre-fabricated orthoses throughout the treatment course. Also, there was no placebo control group to compare results against. Further studies should have two groups, one treated with MLS Laser, the other group with a sham laser. Patients would be blinded as to whether or not they are receiving the actual laser therapy. Ideally, the practitioner would also be blinded as to whether they are actually administrating laser therapy, thus creating a placebo-controlled double-blind study.
Also, typical treatment in the office consists of a session of the robotic head at eight inches away for a prescribed treatment area, followed by the hand held diode over points of maximal tenderness. In order to streamline treatment, only the hand held laser was used in this experiment. While a smaller sample sized allowed all patients to be treated at one location, a larger sample size would likely yield more accurate results. Long-term follow-up should also be better looked at to determine lasting results of the laser therapy, as more than half the subjects in this study did not report for their 8 and 12-week post treatment visit. Would treating other areas such as the tarsal tunnel (tibial nerve and its branches) increase the effect of treatment? All patients were treated at the pre-determined fascial settings of tendinitis. Are these the best parameters for plantar fasciitis?
CONCLUSION
MLS Therapy is an exciting treatment option for musculoskeletal inflammatory conditions. It is a medicine free, pain-free way of treating chronic issues. This study has shown the MLS Laser to reduce the symptoms in 80% of patients suffering from plantar fasciitis. While these results are quite promising, a blinded, placebo-controlled study needs to be performed, ideally with MLS Laser Therapy being the first treatment initiated, and patients need to be followed for a longer period of time.