Since one of the possible ways to use the CO2 laser is to cut soft tissues, it is interesting to note which features distinguish it from the “competition”: the traditional scalpel and electrosurgical scalpel.
Traditional Scalpel:
- Tissue discontinuation with involvement of vessels and nerve endings.
- Need for hemostasis
- Need for a sterile field
- Large surgical volumes
- Need for suture stitches
Healing:
- Cicatrisation is prevalently obtained by first intention
- Cell damage is maximum in the excision spot, moderate in the surrounding areas
- There is foreign body reaction, secondary to the presence of suture stitches
- In veterinary medicine, it is often complicated by secondary infections (auto-traumatism, licking, etc.).
Non-contact or free-contact surgery
Furthermore, there are differences during and after the surgical intervention. During surgery, the use of laser allows the surgeon to have a dry, clean, sterile field, with no need for wide access areas, as this kind of surgery is performed from a distance and not in contact.
Light bleeding and minimal post-operative edema
The main difference from the traditional surgical scalpel consists in bleeding and lymphorrhagia. Using the surgical scalpel, small vessel tamponade is necessary, while, using the laser, small vessels, together with lymph vessels, are self-occluded by wall coarctation. Medium size vessels must be tied in both procedures. This vessel and lymphatic self-obliteration ensures an easier post surgery recovery, with a lower prevalence of fluid collections and oedemas.
No, or fewer stitches required
Finally, dieresis with the surgical scalpel required suture stitches to be used. The stitches stimulate an inflammatory reaction due to the presence of a foreign body and constrict microcirculation. All this slows down repair processes.
The healing of the cut done with a traditional surgical scalpel is prevalently obtained in first intention treatment; cell damage is maximum in the excision spot, but moderate in the surrounding areas; there is a secondary foreign body reaction due to suture stitches and, in veterinary medicine, this mode of operating is often followed by complications due to self-traumatism, licking or poor hygienic conditions.
Traditional scalpel & inflammation
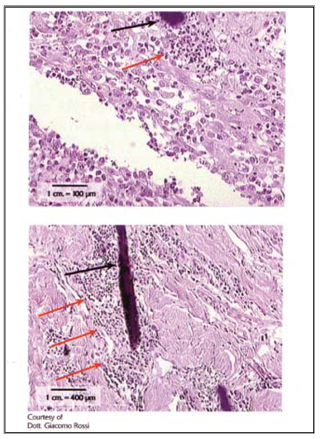
Traditional surgical incision after one day; the histological evidence below, stained with H&E, shows the first phase of the first intention tissue repair process in a cut done with a traditional scalpel.
Stitch Reaction
In the lower part of the picture, we can still see the clot; epithelial proliferative phenomena have not yet started, but the inflammatory infiltrate is very clearly highlighted and substantial in size around the margins of the cut.

Here we can see a foreign body reaction secondary to the presence of a suture stitch, with evidence of the presence, around the suture stitch, of neutrophil granulocytes.
Foreign body reaction due to suture stitch
The histological evidence below shows the foreign body reaction secondary to the presence of a suture stitch, with clearly visible neutrophil granulocytes (red arrows) around the spot (black arrow).
Electrosurgical scalpel and CO2 laser: intra-surgery and post-surgery differences
The first difference consists in the fact that the electrosurgical scalpel, like the traditional scalpel, is a tool that comes into contact with the organ to be treated, and therefore needs larger surgical volumes than the laser.
The electrosurgical scalpel transfers energy to the target tissue using the passage of alternating current. The immediate physical effect of this onto the tissue is similar to the effects of the laser and consists in transforming the energy released into heat, thus causing a thermocoagulating effect onto the tissues around the cutting surface.
Use of alternating current:
- Immediate effect (24-48h) transformation of energy into heat → tissue coagulation, up to 150pm (laser 50pm)
- Deferred effects (5-11 days) alteration of ion exchanges due to inversion of the membrane potential (Na=/K+pump), intracellular edema → varying degrees of hydropic degeneration
Thermocoalgualtion
The electrosurgical scalpel offers more assurance for hemostasis compared to the laser, as it also has an effective action onto small-medium size vessels; this is why the two techniques are almost always used in association. During tissue dieresis, the thermocoagulation effects of the electrosurgical scalpel are much more massive than those induced by the laser and the irreversible thermal damage involves a residual area that may even be ten times larger. Immediate necrosis concerns the cells contacted by the surgical scalpel.
But major differences between the two procedures, when used in combination for tissue dissection, are observed in the post-surgical phase. The electric wave transmitted to the tissue, as in electrocution, is propagated through micro circulation and inverts the membrane potential of the cells around the treated area for a depth of even a few millimeters.
Delay wound healing
This causes a widespread cellular edema, with varying degrees of hydropic degeneration, which delays repair processes.
- The significant differences in tissue repair processes occur between the 2nd and the 5th day –> secondary colliquative necrosis phenomena, that are typical of the electrosurgical scalpel but are absent in the laser, induce a delay in tissue repair.
- The laser scattering phenomenon seems to be capable of inducing the photochemical effect mainly in the residual area. This is translated into a mild anti-inflammatory and biostimulating effect, which is useful to achieve restitutio ad integrum.
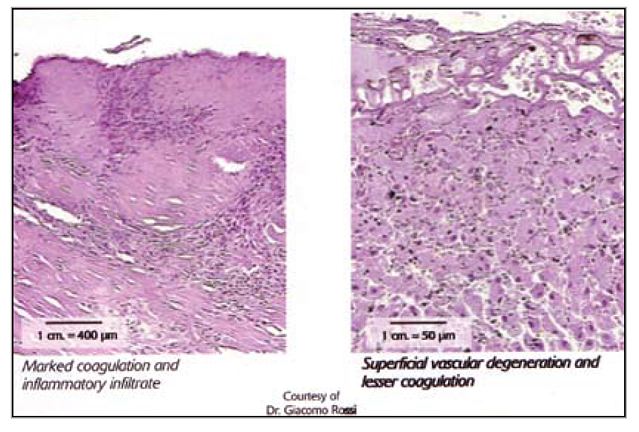
The damage reaches its maximum expression around the 10th-13th day. The repair process occurs by second intention because the marked necrosis provokes the formation of an eschar. Electrosurgical scalpel incision (on the left): the morphological evaluation in H&E highlights the massive coagulation of the residual area. This looks much greater than laser-induced photo-coagulation. In addition, note the presence of inflammatory infiltrate, rarely found in laser dissection. Laser incision (on the right): microscopically starting from the surface, you can see the following areas: vascular degeneration, the residual photocoagulated area, and the underlying healthy area. Please, note the huge difference between the two kinds of equipment as to the magnitude of the residual area coagulation.
Tissue incision by CO2 laser gives better results than surgery with traditional or electrosurgical scalpel. The selectivity and accuracy allowed by the laser beam, as well as the possibility to operate from a distance through small operating breaches, associated with its biostimulating effect not only ensures high safety and efficacy standards, but make up the foundation of minimally-invasive surgery.



